Gastric Bypass Surgery
-
Written by Andrew Proulx, MD | Medically Reviewed by EnhanceMyself Medical Team | Last updated 10/20/2023
- Overview
Overview
What is gastric bypass?
Gastric bypass, also known as a Roux-En-Y gastric bypass (RYGB), is a type of bariatric surgery (weight-loss surgery) performed to aid weight loss in individuals who are severely obese. It is one of the most common and effective types of bariatric surgery.
Cost of gastric bypass surgery
On average, gastric bypass procedures cost between $25,000 to $30,000 according to a JAMA Surgery study. There are several factors that can influence the cost of treatment, such as:
- Your Bariatric Surgeon: The experience of your bariatric surgeon can affect the overall cost. Usually, surgeons with advanced training or specialization charge higher fees.
- Location Matters: Bariatric practices in urban areas with a higher cost of living charge higher fees compared to rural areas.
- Type of Procedure: The costs will vary depending on the type of bariatric procedure (ie gastric bypass, gastric sleeve, etc.).
- Anesthesia: The type of anesthesia, procedure duration, and the qualifications of the anesthesiologist can influence the anesthesia fee.
- Surgical Facility: Different facilities have varying levels of accommodations which can affect the overall price.
- Complexity of Case: Complex bariatric cases that require more advanced techniques and additional time may impact cost.
- Pre and Postoperative Care: This includes consultations, medical tests, medications, and follow-up appointments.
- Insurance: Bariatric surgery may be covered by insurance if it’s deemed necessary and certain criteria are met.
If you are considering gastric bypass surgery, schedule a consultation with an experienced bariatric surgeon near you. This will allow you to discuss your weight loss goals and obtain a better understanding of the specific costs involved.
Are you a candidate?

- Your body mass index (BMI) is 40 or higher
- Your BMI is between 35 and 39.9 (obesity) and you have other health problems such as high blood pressure, type 2 diabetes, heart disease, sleep apnea, osteoarthritis, and more.
Patients must be prepared to make important diet and lifestyle changes before and after surgery. Commitment to making these changes is often required before a surgeon will perform the gastric bypass. If you have any of the following conditions, gastric bypass may not be the right option for you:
- Severe heart failure
- Active cancer treatment
- Drug/alcohol dependency
- Untreated mental health conditions, such as depression or psychosis
- Portal hypertension
- Unstable coronary artery disease
- End-stage lung disease
- Impaired intellectual capacity
- Negative reactions to anesthesia
Benefits of gastric bypass
Gastric bypass is a commonly performed procedure and is considered the “gold standard” for weight loss surgery. Patients who undergo gastric bypass are less hungry than before the procedure, because their stomachs stop producing ghrelin, the hormone that stimulates appetite. There are other health benefits, including the reversal or improvement of underlying health conditions caused by obesity such as:
- High cholesterol
- Heart disease
- Type 2 diabetes
- Non-alcoholic fatty liver disease
- Obstructive sleep apnea
Procedure overview
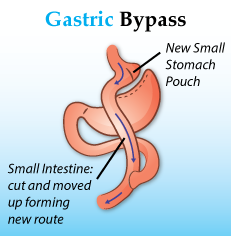
During an RYGB, the surgeon will use staples to create a small pouch with the upper portion of the stomach. This pouch is roughly the size of a walnut and can hold around 1 ounce of food.
The surgeon then connects the pouch to the lower part of the small intestine. This allows food to “bypass” most of the stomach and small intestine, resulting in fewer calories and nutrients being absorbed.
In most cases, the RYGB is performed laparoscopically, using long, thin instruments inserted into small incisions made in the abdomen. This type of surgery offers quick recovery times and is less invasive than open surgery, which requires large incisions.
Safety information
Every surgical procedure comes with side effects and risks. It is important to discuss these with your doctor and make the best-informed decision for yourself. Some potential risks include:
- Malnutrition: Vitamin and macronutrient deficiencies can occur due to changes in the stomach and intestines’ ability to absorb nutrients.
- Small bowel obstruction: This is most often caused by an internal hernia, or when the bowel juts out through a defect created from surgery in the abdominal cavity.
- Dumping syndrome: Dumping syndrome occurs when food moves too quickly from the stomach into the small intestine; this causes diarrhea, nausea, vomiting, lightheadedness and flushing.
- Anastomotic Leakage: Leaks from where the stomach and/or intestines are sewn together can occur, spilling digestive juices and food into the abdomen. Most leakages develop within 3 days of surgery.
- Anastomotic stenosis: Also known as a stricture, this can occur when the new connection between the stomach pouch and the small intestine narrows.
- Gastrogastric fistula: This complication occurs when an abnormal tract forms between the new stomach pouch created during gastric bypass, and the old stomach remnant.
- Stomach or intestine marginal ulcers: These are one of the most common complications to develop after gastric bypass.
Recovery time
Most patients spend one to three nights in the hospital recovering.
It takes about six to eight weeks to fully recover, although many are able to return to work after two to three weeks.
After surgery, patients must make significant lifestyle changes to best recover and maintain their weight loss. It is most important to change food intake, since the stomach can now only hold a few ounces. Small meals that are low in sugar and fat are best.
You will also need to take daily dietary supplements to replace the vitamins and macronutrients that are no longer absorbed by the intestine.
What type of results to expect
Following gastric bypass surgery, a study found that 80% of patients lose more than 70% of their excess weight over two years. In order to maintain this weight loss over time, patients should:
- Eat a healthy, well-balanced diet
- Drink plenty of water
- Take vitamin supplements (multivitamins, calcium, vitamin D, vitamin B-12 and iron)
Alternatives to gastric bypass
There are a number of non-surgical weight loss programs that may help manage chronic obesity; however, they take time and may not work for everyone. In cases where weight loss and lifestyle changes have failed, there are other surgical options besides gastric bypass.
- Gastric balloon: A silicon balloon is placed in the stomach to take up volume; patients feel fuller and, as a result, will eat less food. This procedure is recommended for patients with a BMI of 30 to 40. The balloon will remain in place for six months, and patients may lose up to 15% of their body weight.
- Aspiration therapy: A small tube with an access port is placed into your stomach by an endoscopy specialist; after 2 weeks, the port is connected to the surface of the skin, and patients can empty up to 30% of calories from the stomach after each meal. This procedure is recommended for patients with a BMI greater than 35, and they may lose up to 16% of their body weight during the first year.
- Sleeve Gastroplasty: During a gastric sleeve, the stomach is stitched to reduce the volume by 70%. The stitches typically last 1 year before the body reabsorbs them. Patients may lose up to 20% of their body weight from this procedure.
- Adjustable Gastric Banding: An adjustable band is placed around the top part of your stomach, creating a small stomach pouch that holds less food. The band can be tightened or loosened by the addition or removal of sterile saline through a device under the skin. An example of gastric banding is the LAP-Band System.
EnhanceMyself.com relies on sources such as professional medical organizations, government agencies, academic institutions, and peer-reviewed scientific journals to write it’s articles. Learn more about how we ensure our content is accurate, in-depth, and unbiased by reading our editorial guidelines.
*Medical Disclaimer: This website does not provide medical advice. Read more.

