Cataract Surgery
-
Medically Reviewed by Joseph Christenbury, M.D. | Last updated 10/17/2023
- Overview
Overview
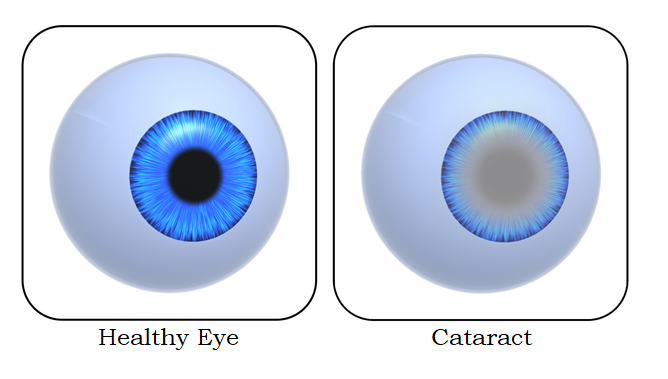
What is a cataract?
A cataract is a gradual clouding of the lens in the eye that can cause a variety of visual defects and losses. The lens, located in the front part of the eye, transmits and focuses light onto the retina at the back of the eye. The lens is dynamic and can change its shape to focus on objects at various distances. The eye and its lens are made up mostly of proteins and water. As we age, the proteins may clump together creating areas of cloudiness and opacity. That condition is what is referred to as a cataract.
The prevalence of cataracts is expected to rise over the next 30 years. The U.S. National Eye Institute estimates that the number of Americans with cataracts will double by the year 2050
Topics covered on this page
- Cost of cataract surgery
- Cost of different cataract procedures
- Symptoms of cataracts
- Testing and diagnosis
- Cataract treatment options
- IOL options
- When to expect results
Cost of cataract surgery
The average cost of cataract surgery can range between $1,808 and $2,866 per eye according to Medicare. The journal of Clinical Research in Ophthalmology found similar numbers with the average cost being $2,526 per eye. However, these numbers only include the cost of surgery and the facility fee. There are several other factors that can influence the cost of your procedure, such as:
- Your Ophthalmologist: The experience and reputation of the ophthalmologist performing your procedure can affect the cost. Highly skilled ophthalmologists often charge a premium for their services.
- Location Matters: Where you live can impact the cost of cataract surgery. Generally, healthcare expenses tend to be higher in urban areas and regions with a higher cost of living.
- Surgical Technique: The surgical technique used can affect the overall cost. Traditional cataract surgery (extracapsular cataract extraction or ECCE) is typically less expensive than more modern methods like phacoemulsification or laser-assisted cataract surgery (LACS).
- Choice of Intraocular Lens (IOL): In cataract surgery, the natural lens of the eye is replaced with an artificial intraocular lens (IOL). The type of IOL you select can impact the cost. Standard monofocal IOLs, which provide clear vision at one distance, are usually covered by insurance. However, premium IOLs like multifocal or toric lenses, which correct astigmatism and offer a broader range of vision, may require an additional out-of-pocket expense.
- Surgical Facility: These fees cover the usage of the operating room and other associated services.
- Pre and Postoperative Care: This includes consultations, medical tests, medications, and follow-up appointments.
- Insurance: Generally, medical insurance covers cataract surgery as it’s considered a medically necessary procedure. However, the specifics of your insurance plan may impact coverage details. Typically, insurance covers the basic costs of the procedure such as surgeon and facility fee, and standard IOLs.
When taking all these factors into consideration, the total cost of catract surgery can range between $3,500 to $7,000 per eye.
If you are considering cataract surgery, schedule a consultation with a board-certified ophthalmologist near you. This will allow you to discuss your vision goals and obtain a thorough understanding of the specific costs that pertain to your individual case.
Cost of different cataract procedures
Below are the average costs for different types of cataract treatments:
- Traditional Cataract Surgery (ECCE): $3,000 to $5,000 per eye.
- Phacoemulsification Cataract Surgery (Phaco): $3,500 to $6,000 per eye.
- Laser-Assisted Cataract Surgery (LACS): $4,000 to $8,000 per eye.
- Premium Intraocular Lenses (IOLs): $1,000 to $4,000 per eye.
Symptoms of cataracts
Cataracts can lead to a variety of vision problems that get worse as time goes on. If you happen to notice any of the following changes in your vision, it’s a good idea to reach out to an eye care specialist for a proper assessment. Some common signs of cataracts might include:
- Blurry or Hazy Vision
- Difficulty Seeing Colors Clearly
- Increased Sensitivity to Bright Lights
- Challenges Seeing in the Dark
- Seeing Double Images
- Frequently Changing Glasses Prescriptions
- Struggles with Reading or Close-Up Tasks
- Trouble Judging Distances
Its important to keep in mind, cataract symptoms can differ from person to person, and cataracts tend to develop gradually. Regular eye check-ups with an eye doctor can help in the early detection of cataracts and help determine the appropriate treatment plan.
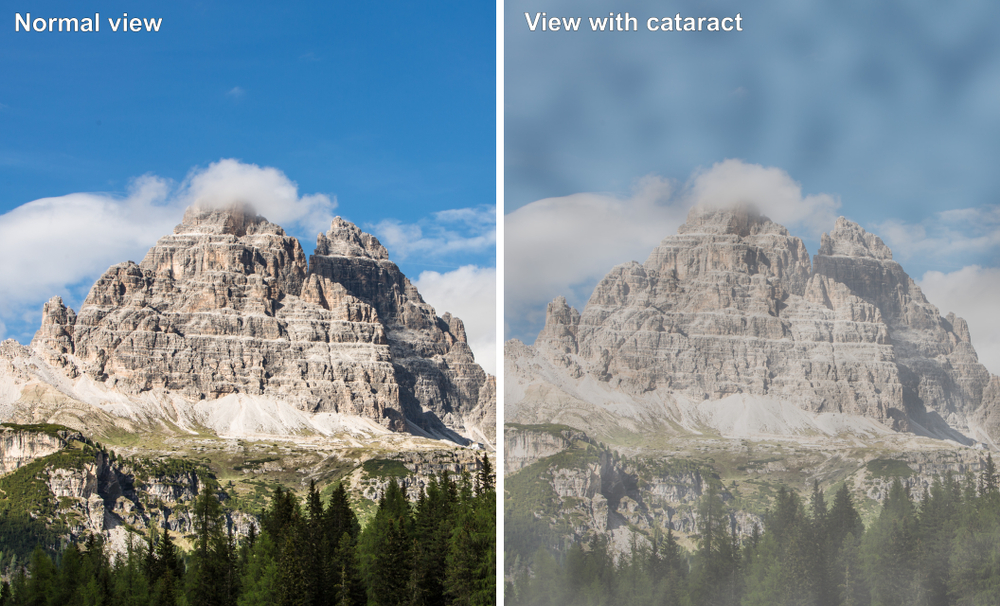
An illustration of normal vision vs. cataract
Testing & diagnosis
Ophthalmologists and optometrists have several tests at their disposal to diagnose cataracts. These include:
- Visual acuity tests: These measure how well you can see at varying distances. Your doctor will ask you to read out loud a set of letters on an eye chart. This test is done using one eye to look at the letters while the other eye is covered. There are various sizes of the letters to determine whether your vision is impaired.
- Slit lamp examination: This involves using a “slit-lamp” – which is a type of microscope specially designed for looking at the front part of the eye – to examine your eye under magnification with good lighting. Slits in the light allow the doctor to see even tiny abnormalities within the structure of the eye.
- Pupil dilation: The doctor uses special drops to dilate your eyes causing the pupil to increase in size, giving the doctor a clear view into the lens of the eye. With this examination, the doctor can also get a good look at the retina (fundoscopic exam) to look for other problems that may be affecting your vision.
Cataract treatment options
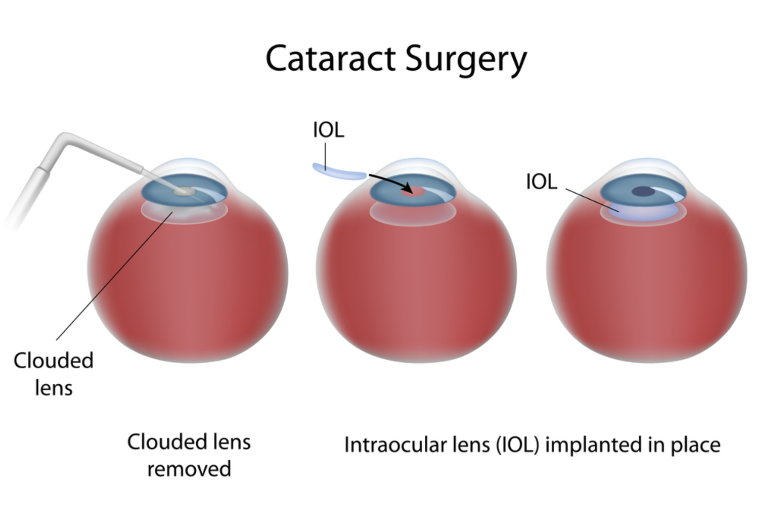
Cataract extraction is the primary course of action when treating vision loss caused by cataracts. Most doctors recommend this surgery when cataracts start to affect vision and quality of life.
With cataract surgery, the lens of the eye is replaced with an artificial lens called an intraocular lens (IOL) implant. In the rare cases when the surgeon does not deem it safe to implant an IOL, the cataract is removed and the patient is prescribed glasses or contact lenses to correct their vision.
There are essentially two types of cataract surgery to choose from: traditional or laser.
Traditional Cataract Surgery – Phacoemulsification
Most cataract procedures today involve the use of an ultrasound device to break up the cloudy lens into small pieces, which are then removed by suction from the eye. This is known as phacoemulsification, or phaco. During phaco, a topical or local anesthetic is applied to the eye before treatment to minimize any discomfort or pain associated with the procedure. Once the cataract has been removed, an IOL is placed into the remaining lens capsule to restore vision. Depending on the type of IOL used, a larger incision may be required, which typically requires closing the incision with sutures. If using a smaller, foldable IOL, sutures are usually not needed. This is performed as an outpatient procedure that usually requires less than 30 minutes to perform. Typically the patient spends only a few hours at the surgical center.
Laser Cataract Surgery
Laser cataract surgery, also referred to as the “bladeless” technique, is a new form of surgery that uses femtosecond laser technology to treat cataracts. Harnessing the technology responsible for the advanced accuracy and safety of LASIK surgery, laser cataract surgery improves the precision of treatment. Laser cataract surgery can result in better outcomes than traditional surgical methods for certain patients, particularly those with corneal astigmatism.
As with other types of cataract surgery, this is an outpatient procedure. Patients are awake during the procedure, requiring only anesthetic eye drops to numb the eye. Prior to making any incision in the cornea, the laser creates an opening in the front of the lens capsule, called the capsulorhexis and uses laser energy to soften and break apart the cataract, making removal easier.
Next, the surgeon creates an incision in the cornea to enter the front of the eye. In traditional cataract surgeries, this incision is created with a handheld surgical blade. A benefit of laser-assisted cataract surgery is that the femtosecond laser is used to create the incision.
Once the surgical instruments are inside the eye, the cloudy lens is removed in small pieces. Finally, the eye’s natural lens is replaced with an IOL. This step is performed in the same manner as in traditional surgery.
IOLs – which option is best for you?
There have been significant advancements in the field of intraocular lenses since they were first approved by the FDA in the early 1980s. Cataract surgery patients can now select from a variety of traditional and premium IOL options.
Traditional (monofocal) IOLs
A traditional IOL is made of silicone or acrylic and designed to cater to vision at one focal distance; as such, they are known as “monofocal.” These can be chosen as either for near or distance vision. Most people opt for distance vision and use reading glasses for near vision if needed. Traditional monofocal IOLs are the cheapest and most commonly used variety for cataract surgery.
Premium (multifocal and accommodative) IOLs
Cataract surgery patients who want clear focusing across multiple distances will need to opt for a premium IOL. Multifocal IOLs offer clear vision at two focal distances, near and far; unfortunately, vision between the two points will not be corrected. Accommodative IOLs are similar to multifocal IOLs in that they cater to more than one focal point, but unlike multifocal lenses, they do not have fixed distance focal points. As the name implies, accommodative IOLs accommodate your vision across all distances. This is most like the natural lens of the eye.
Toric IOLs
Cataract surgery patients who also suffer from astigmatism may opt for a Toric IOL. Like multifocal IOLs, Toric IOLs can correct near-sightedness and farsightedness, while also correcting the irregular shape of the cornea that causes astigmatism. These are considered to be a premium lens.
When to expect results
After cataract surgery, you can expect to notice improvements in your vision within 24-48 hours, but it may take up to two weeks for your eyes to fully adjust to the new implants. For most patients, they can resume their normal activities as soon as the day after the procedure. Right after surgery, your vision may initially appear somewhat blurry or in soft focus.
EnhanceMyself.com relies on sources such as professional medical organizations, government agencies, academic institutions, and peer-reviewed scientific journals to write it’s articles. Learn more about how we ensure our content is accurate, in-depth, and unbiased by reading our editorial guidelines.
*Medical Disclaimer: This website does not provide medical advice. Read more.